
TOTAL HIP ARTHROPLASTY
TSUJI ORTHOPAEDIC INSTITUTE
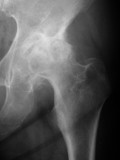
PAINFUL LESIONTotal hip arthroplasty (THA) is the gold standard of treatment in these patients. I have corrected the leg length discrepancy and in just one year after surgery in this patient on this x-ray, the shaft of the femur is coming back to have normal bone quality.
Description about THA
 Total hip arthroplasty (THA) also called as total hip replacement (THR) is a surgical procedure to reconstruct the arthritic or destructed hip joint using artificial prostheses. This surgical treatment is performed on people who are suffering from severe hip pain, walking disability, disabling joint stiffness and reduced activity of daily living. The head and neck of the femur (thigh bone) and the inner surface of acetabulum (hip socket) are resected or trimmed and replaced with total hip prosthesis.
Total hip arthroplasty (THA) also called as total hip replacement (THR) is a surgical procedure to reconstruct the arthritic or destructed hip joint using artificial prostheses. This surgical treatment is performed on people who are suffering from severe hip pain, walking disability, disabling joint stiffness and reduced activity of daily living. The head and neck of the femur (thigh bone) and the inner surface of acetabulum (hip socket) are resected or trimmed and replaced with total hip prosthesis.
Modern common total hip prosthesis is composed of four components as follows.
 1. Stem - femoral implant, a stiff prosthesis inserted into the femoral canal
1. Stem - femoral implant, a stiff prosthesis inserted into the femoral canal
2. Head - ball on top of the femoral stem for articulation
3. Cup - acetabular component or acetabular shell fixed into the acetabulum (socket)
4. Liner - inner material (ceramic or polyethylene) placed inside the metal cup




Annual numbers of THA's
Approximately 300,000 hip arthroplasty surgeries are performed annually in the United States alone and 70,000 in Japan. Just less than 100,000 hip arthroplasties were performed when I was in the U.S. in 1986 through 1987, so three times more people are undergoing total hips than twenty years ago including younger patients as well than before.
Indications for THA






Purposes and benefits of THA
The primary purpose of total hip arthroplasty is to relieve or alleviate hip pain most often at groin and thigh. When there is a joint stiffness, we want to restore range of motion of the hip joint so that the patients can wear socks by themselves and cut the toe nail by themselves. By relieving the hip pain, the patients can ambulate more and their walking and sporting ability increases. Before the operation, they tend to prevent from walking in distance, but after the operation they would enjoy walking around in the shopping mall or enjoy bicycle ride under the sunny sky. Exercise in the swimming pool is also recommended. Some people without much obesity are allowed to play low-impact sports like tennis (doubles only!) or golf. (But always keep in mind preservation of polyethylene and prevention of poly wear is very important! It is better to refrain from mountain climbing or jogging.) Preoperatively, you used to prefer to stay alone in a quiet place and then the quadricep muscles show signs of atrophy which you notice when you touch and compare the muscles three to four inches proximal above the knee cap. If you get a successful operation, you will be able to use the muscles more and then you will get improvement of muscle strength. We would want to restore the leg length discrepancy (leg shortening) as much as possible if there is any. Limping will usually get better or disappear by pain relief, recovery of the muscle strength, improvement of the range of motion and correction of the leg length discrepancy.
We are now having the benefits of minimally invasive total hip arthroplasty at more facilities. The recovery time after total hip is shorter and postoperative muscle power loss is minimal.
I have made consecutive thumbnails of the photos of minimally invasive total hip arthroplasty procedure. More explanations about minimally invasive total hip arthroplasty (MITHA) are written here.












Ambulation four days post MITHA
(HDTV wmv)
#1. Deep Vein Thrombosis (DVT)
The most common complication after total hip arthroplasty nowadays is the formation of blood clots in the deep thigh vein near the surgery site. This is called deep vein thrombosis or thrombophlebitis. When this occurs your affected limp swells and it may hurt. The clots have the risk of traveling through the vein and may cause pulmonary infarction when they reach lung. This could be fatal if it's serious so we have to keep an eye on this problem carefully and the earlier we find the better the response to treatment. We prevent this by subcutaneous injection of fondaparinux sodium ( ArixtraTM), but once this occurs, intravenous drip infusion of heparin works best at an early stage. Although heparin does not dissolve blood clots that have already formed, it prevents the enlargement of the clots and further serious problems. You may return from the operating room with anti-embolism stockings for reducing the risk of DVT. Pulling the soft tissue too hard during the surgical maneuver which may damage the fragile vein or too much post-operative limb immobility are among the important risk factors that I think. Race is also a risk factor and Caucasians get more DVT than Orientals. I got the feeling during operation in the U.S. that the viscosity of the blood is higher and their blood tends to coagulate much earlier than the Japanese even at the time of surgery.
#2. Dislocation
There are two directions of hip dislocation after surgery. The surgeons have basically two ways of approaches, anterior and posterior. I would like all patients who underwent total hip surgery to learn their own approach they got at the time of surgery.
With an anterior approach, hip may dislocate when you externally rotate the limb with abduction. With a posterior approach, it may dislocate when you internally rotate the limb with adduction and flexion. The dislocation rate is higher with the posterior approach. This usually happens when you take a squatting position. When you have unfortunately dislocated the hip, remember the positions and the directions of dislocation and keep away from that. When we surgeons place the cup covering well over the femoral head and suture the joint capsule tightly choosing the anterior approach with the femoral head with larger diameter, the dislocation rate actually decreases. I personally haven't had the dislocated patients after THA for five years with these cautions.
#3. Infection
There are two types of infections, early infection and late infection. Early infection is affected by the intra-operative environment. Early infection rate reported to have reached up to 3 to 5 % before. It is now reduced down to 0.5 to 1% because ultra-clean OR (laminar flow room) is available where high-efficiency particulate air (HEPA) filters are used to remove particles larger than 0.3 micron in size. Since the size of bacteria is 0.5 micron or more (average 0.8 micron), the HEPA filter can signifcantly reduce the numbers of airborne bacteria. I also wanted to remove more airborn bacteria before we enter the ultra-clean OR, I had placed HEPA filters at the adajacent entrance hall to the ultra-clean OR and the corridor in the OR area and the adjacent central steril supply (CSS). Moreover, I had placed the surgical area at the top floor of the hospital building, where entrance is restricted to the hospital staffs and thus minimizing the traffic in and out of the OR to an extreme point. The infection rate is reduced also because we carefully wash the surgical site with "ZIMMER Pulsavac Plus Wound Debridement System", we drape surgical skin area with "3M Ioban 2 Antimicrobial Incise Drapes" and also the operation time is getting shorter than before. Late infection is more affected by the patient status. Patients with rheumatoid arthritis and diabetes mellitus have two times higher risk of infections after total hip arthroplasty. If you have signs of pneumonia or urinary tract infection or gingivitis, it is recommended to get the treatment early to avoid late infection.
#4. Fracture
Postoperative thigh pain is minimal when the stem is tightly fixed in the medullary canal of the femur. For this purpose, the surgeon attempts to place as large stem as possible there. When we go to a too large stem, fracture of the femur may occur. If this happens, we place wires or cables around the femur and fix the fracture.
#5. Nerve palsy
Cautious surgeons do not usually damage the nerves, even though nerve palsy may occur when the surgeon tries to extend the lower extremity more than an inch which is often associated with later recovery.
#6. Metal allergy
Some people may be allergic to certain kind of metals such as nickel, cobalt and chrome. Titanium is one of the least allergic metals to human body among those used for prosthetic implants. Although its incidence is much less than over the skin, if allergic reaction may occur inside the bone, we may have to remove it and fix a new component with cement.
#7. Trochanteric bursitis
Other than the metal allergy, trochanteric bursitis may induce local inflammation. This inflammation usually subsides with local injection of corticosteroids.
#8. Loosening and wear
Loosening occurs both around the femoral stem and around the acetabular cup. When the prosthetic implants were fixed with the old cementing technique, loosening rate was five to seven percent at ten years after surgery and fifteen percent at fifteen years and thirty percent at twenty years. Now more and more surgeons are using the cementless fixation with which we expect bone-ingrowth into the porous-coated surface of the implant materials, the loosening rate went down to three percent in fifteen years. We now have a hydroxyapatite coated porous surface to achieve better bone-ingrowth. Porous surface is not versatile because some people have metal allergy even in the bone canal. Cementing technique has also advanced and we have better longevity than before even when cement-fixed.
The last problem we are facing is the wear of the polyethylene liner. In recent years we are able to use the cross-linked ultra-high molecular weight polyethylene (cross-linked UHMWPE). Its wear resistance is five-fold stronger in laboratory hip-simulator studies than the standard UHMWPE. However, there are conflicting reports on "in vivo" studies. Some numbers of retrieval studies have some negative comments on the cross-linked UHMWPE, but I think the UHMWPE were retrieved from failed cases rather than from the good cases. How the cross-linked UHMWPE behaves in vivo is the ultimate test whose answer we still don't know yet, but it looks like better in my experience. I had revised a conventional UHMWPE liner which had been worn and failed after six years post-operatively to a new cross-linked UHMWPE, without revising the acetabular shell. The cross-linked UHMWPE has no sign of wear right now after six years in the same patient with the same activity level, so I am expecting the overall clinical longevity would similarly be promising.
For highly active patients, even the cross-linked UHMWPE may not be strong enough to last through the period of decades. For improving the polyethylene wear problems, new ideas of bearings like ceramic-on-ceramic or metal-on-metal coupling arose for such patients. Some new progress about ceramic-on-ceramic articulation is described later.
And finally, it is also very important to place the implants in ideal position for achieving a satisfactory longevity.
Natural course of osteoarthritic hip without total hip arthroplasty
There are three kinds of courses.
Group I: Slowly progressive type
There are few changes on x-ray follow-ups even when I keep observing them for ten years at outpatient clinic. These patients are usually fairy disabled already and are less active during the follow-up period.
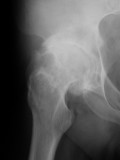
Group II: Moderately progressive type
The people in this group are most common. The x-ray appearance of the hip joint deteriorates little by little when they return to clinic. The joint space shows progressive narrowing to the point where there is none in some years.
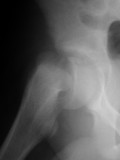
Group III: Rapidly destructive type
Just in three to six month, femoral head may collapse and the patients may have severe hip pain and often very difficult to walk. This is sometimes associated with patients with osteoporosis and obesity.
We have to pay close attention to these people in group II. Some people don't complain hip pain so much. But on physical examination, their gluteus medius and quadriceps show muscle weakness and their hips may be stiff. Femur (thigh bone) also shows atrophy and shortening on x-ray appearance. The reason why they say they have little pain on ambulation is because they choose to refrain from harder activities than they can afford to, that means you have reduced walking distance. Stiff hips associated with shortened limb will affect other parts of your body like contralateral knees and low backs. It is kindly advised to have the first problem fixed before you have secondary problems at other parts of your body in this group of people. By means of x-ray follow-up at outpatient clinic, we know to which group you belong.
Autologous re-infusion (transfusion)
400ml of blood is pooled preoperatively and intra-operative autologous re-infusion (transfusion) is made using "Stryker CBCII Constavac Blood Conservation System". Along with the anesthesia controlled in hypotension, homologous transfusions are avoided in most cases.
From what materials are the implants made?
This is a frequently asked question from the patients who undergo total hip arthroplasty.
 1. Stem is made from titanium alloy or cobalt-chrome(-molybdenum) alloy. Cobalt-chrome-molybdenum alloy (Vitallium) is stiffer than titanium alloy, so when we had encountered stem fractures decades ago, it emerged as the strongest and most ideal material. Titanium alloy is less stiff than cobalt-chrome alloy but has much better compatibility with bone. Modern technology has introduced computer assisted design (CAD) and computer assisted manufacturing (CAM), this can be so made that no more stem fractures may occur and now titanium alloy is becoming one of the most suitable materials for the femoral stem.
1. Stem is made from titanium alloy or cobalt-chrome(-molybdenum) alloy. Cobalt-chrome-molybdenum alloy (Vitallium) is stiffer than titanium alloy, so when we had encountered stem fractures decades ago, it emerged as the strongest and most ideal material. Titanium alloy is less stiff than cobalt-chrome alloy but has much better compatibility with bone. Modern technology has introduced computer assisted design (CAD) and computer assisted manufacturing (CAM), this can be so made that no more stem fractures may occur and now titanium alloy is becoming one of the most suitable materials for the femoral stem.
 2. Head has been made from cobalt-chrome alloy because it used to have been the hardest material for prosthesis. But there is a problem that its surface gets abraded and roughens in years, which accelerates polyethylene wear of the acetabular liner. Now, the second or the third generation ceramic is a better wear resistant material and more orthopaedic surgeons are in favor of it.
Since the ceramic is glass compound, the first generation alumina ceramic that was used in the 1970's for orthopaedic implants was brittle and some breakages were seen occasionally. Its hardness on Mohs scale is said to have been 8.5 or less which was below corundum (=sapphire or ruby) whose hardness on Mohs scale is 9 (Vickers hardness 2085 Hv) and also the strength was not satisfactory enough for clinical use. Now we have second generation zirconia ceramic and third generation alumina ceramic. The second generation zirconia ceramic (Mohs scale 7.5 and Vickers hardness 1300 Hv) is becoming my preference now when I use it with cross-linked polyethylene, because its hardness is enough against polyethylene and its strength (=resistance to breakage), which is another issue than hardness, is two times stronger (zirconia=9.2MPam1/2, alumina=4.8MPam1/2) than the third generation alumina ceramic and there has not been any breakage when used with poly-liner in ten years of clinical use so far. Since the surface of the zirconia head (Ra=0.006 micro meter) is fifteen-times smoother than cobalt-chrome head (Ra=0.091 micro meter), the clinical wear rate of polyethylene with zirconia head (0.7mm/10yrs) is approximately 1/3 when compared with usage with cobalt-chrome head (2mm/10yrs). And the long term abrasion over its surface is much less than cobalt-chrome head. If we choose ceramic-on-ceramic articulation, the material must have enough hardness on each side. In that case, the third generation alumina ceramic is preferable because its hardness is right next to diamond which means its Mohs scale is 9.5 (Vickers hardness 2300 Hv). The resistance to wear is 4000 times better than the metal-on-polyethylene bearing and 1500 times better than ceramic-on-polyethylene bearing. It still has the disadvantage of fragility, but the clinical study had revealed that the clinical failure rate had come down to an acceptable level so far as described below.
2. Head has been made from cobalt-chrome alloy because it used to have been the hardest material for prosthesis. But there is a problem that its surface gets abraded and roughens in years, which accelerates polyethylene wear of the acetabular liner. Now, the second or the third generation ceramic is a better wear resistant material and more orthopaedic surgeons are in favor of it.
Since the ceramic is glass compound, the first generation alumina ceramic that was used in the 1970's for orthopaedic implants was brittle and some breakages were seen occasionally. Its hardness on Mohs scale is said to have been 8.5 or less which was below corundum (=sapphire or ruby) whose hardness on Mohs scale is 9 (Vickers hardness 2085 Hv) and also the strength was not satisfactory enough for clinical use. Now we have second generation zirconia ceramic and third generation alumina ceramic. The second generation zirconia ceramic (Mohs scale 7.5 and Vickers hardness 1300 Hv) is becoming my preference now when I use it with cross-linked polyethylene, because its hardness is enough against polyethylene and its strength (=resistance to breakage), which is another issue than hardness, is two times stronger (zirconia=9.2MPam1/2, alumina=4.8MPam1/2) than the third generation alumina ceramic and there has not been any breakage when used with poly-liner in ten years of clinical use so far. Since the surface of the zirconia head (Ra=0.006 micro meter) is fifteen-times smoother than cobalt-chrome head (Ra=0.091 micro meter), the clinical wear rate of polyethylene with zirconia head (0.7mm/10yrs) is approximately 1/3 when compared with usage with cobalt-chrome head (2mm/10yrs). And the long term abrasion over its surface is much less than cobalt-chrome head. If we choose ceramic-on-ceramic articulation, the material must have enough hardness on each side. In that case, the third generation alumina ceramic is preferable because its hardness is right next to diamond which means its Mohs scale is 9.5 (Vickers hardness 2300 Hv). The resistance to wear is 4000 times better than the metal-on-polyethylene bearing and 1500 times better than ceramic-on-polyethylene bearing. It still has the disadvantage of fragility, but the clinical study had revealed that the clinical failure rate had come down to an acceptable level so far as described below.
The heads are placed over the femoral stems like this.
 3. Cup is made from titanium alloy because bone ingrowth over the surface of acetabular component is excellent with this material.
3. Cup is made from titanium alloy because bone ingrowth over the surface of acetabular component is excellent with this material.
 4. Conventional liner is mostly made from (cross-linked) ultra-high molecular weight polyethylene. There have been advancements with all of three components above since the practical introduction of total hip arthroplasty by Charnley in 1961, only polyethylene ensued for decades and could not meet the demands of young active patients. The last biggest problem we encounter with the total hip arthroplasty with young or obese patients is wear of polyethylene. Polyethylene wear is the cause of osteolysis around the prostheses with subsequent aseptic loosening, and once the osteolysis occurs, you will get a painful hip again and the canal made by the osteolysis is also difficult to repair for the orthopaedic surgeons.
4. Conventional liner is mostly made from (cross-linked) ultra-high molecular weight polyethylene. There have been advancements with all of three components above since the practical introduction of total hip arthroplasty by Charnley in 1961, only polyethylene ensued for decades and could not meet the demands of young active patients. The last biggest problem we encounter with the total hip arthroplasty with young or obese patients is wear of polyethylene. Polyethylene wear is the cause of osteolysis around the prostheses with subsequent aseptic loosening, and once the osteolysis occurs, you will get a painful hip again and the canal made by the osteolysis is also difficult to repair for the orthopaedic surgeons.
In last fifteen years in Europe, there were successful reports on ceramic-on-ceramic bearing articulation especially from Germany. As the Food and Drug Administration (FDA) approved Investigational Device Exemption (IDE) protocol, modern ceramic-on-ceramic total hip arthroplasty was started in 1997 and approved in 2003, one year after approval of metal-on-metal in 2002. The results of the Wright's LINEAGE ceramic-on-ceramic hip system revealed that the old issue of ceramic fracture incidence went down to 6/1700 (0.4%) by using stronger third generation alumina, and the problems of loosening rate had decreased down to 8/1700 (0.5%). Reduction of the loosening rate is coming from the improvement of the ceramic fixation method like fixing the ceramic liner along with the porous acetabular socket with improved porous-ingrowth fixation. It is also known by the experimental study that ceramic debris behave better than metal or polyethylene debris in the tissue, which will contribute to smaller incidence of osteolysis and subsequent loosening. And most of all, the wear resistance of ceramic-on-ceramic articulation is 4000 times better than the metal-on-polyethylene articulation. Although mechanical strength and durability of the ceramic liner in long-term clinical use is not established yet, this material is a new hopeful option for young and active high-demanding patients.



History of total hip arthroplasty
I was fortunate enough to be given a chance to present my research results (about AVN) at scientific exhibit at the 54th American Academy of Orthopaedic Surgeons at San Francisco in January, 1987. At the entrance to the Academy Meeting, I was surprised to see all these panels. Famous implants were all displayed at one place at one time and they were all real! This is exactly the history of total hip arthroplasty!

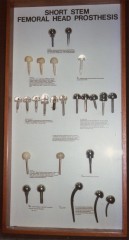





Early form of hip joint reconstruction was initiated with interpositional arthroplasty with soft tissue of the body by Ollier in 1885. Other materials like fascia and skin were also tried later. Cup arthroplasty was started by Smith-Petersen in 1923 using glass mold first. He tried Pyrex and Bakelite and finally came to Vitallium which was rigid and caused fewer problems. Many of the cup arthroplasties failed at the prosthetic-bone interface. This led to the idea of tighter fixation with a stem like short stem femoral head prosthesis (Judet, 1943) and long stem femoral head prosthesis (Thompson, 1950; Austin Moore, 1952) with which other materials like ivory and acrylic were tested before metallic implants. But satisfactory fixation was not achieved with these methods.
The prototype of total hip arthroplasty was done by Phillip Wiles in 1938. This was a metal-to-metal (stainless steel) short neck total hip replacement. In 1961, Sir John Charnley documented an article in the Lancet entitled "Arthroplasty of the Hip - A New Operation." He used cement fixation for prostheses and used a smaller diameter femoral head to acquire low-friction contact between the femoral head and socket and achieved a practical success with long term survival rate. With his contribution, total hip arthroplasty had become the real worthwhile medical treatment rather than a medical curiosity. There were developments in cement fixation stems, but loosened cemented stems were difficult revise when failed. New types of rigid fixations like press fit fixation and porous fixation with bone-ingrowth on to the surface of metal coated stems were among the orthopaedic surgeons' interest. Now there is a consensus that porous-coated femoral implant is favorable for patients with quality bone and cement fixation for osteoporotic patients. I hope the next generation progress in the history will be seen in the advancement of the quality of the liner inside the acetabular shell.
SITE MAP
#HOME-Dedication
#PAINFUL LESION
-Osteoarthritic Knee-Minimally Invasive Total Knee Arthroplasty(Full Flexion Knees)-10yr. F/U-Intra-Op. Photo
-Osteoarthritic Hip-THA(Video movie)-Cemented THA-Minimally Invasive Total Hip Arthroplasty
-Acetabular Dysplasia-JSN-Acute Destruction-Dial Osteotomy-8yr. P.O.-Recent Development
-Humeral Head Fracture-DJD Shoulder-Humeral Head Prosthesis
-Cuff Tear Arthropathy-RCT-Cuff Repair
#TOUR
-Minneapolis-Sears Tower-Skyscrapers-Stream of Lights-Niagara Falls-The Lady-U of M-OR-Mt. Rushmore-AAOS-LA from Hollywood-Walt Disneyland-Grand Canyon-Downtown Minneapolis-Kind Doctor-Linda
#LOCATION(Location-Map by Its-mo Guide Map by MapFan)